
A blog post by Clara Schlösser, Policy Implementation Officer- HCWH Europe.

Single-use medical devices are a common feature in hospitals, including maternity and paediatric wards. However, their widespread use contributes to significant waste and environmental challenges, exacerbating the plastic pollution crisis. One of the goals of the Born Green Generation initiative is to reduce the reliance on unnecessary plastics. While some medical devices are essential and unavoidable, there is an opportunity to make them more sustainable. This is where reprocessing comes in.
Reprocessing is the process of cleaning, disinfecting and sterilising formally labelled single-use medical devices. They can then be safely reused, thereby extending their life and reducing the need to continually produce new single-use devices. This helps to reduce the overuse of plastics and offers a more sustainable alternative.
The Danish Ministry of Health has announced a significant legislative change that will come into force on 1 January 2025. Following successful examples in Germany and the Netherlands, the new executive order will allow the reprocessing of medical devices labelled as single-use. This change, which was initially advocated for several years ago by Aarhus University Hospital which is located in the Central Denmark Region - and one of Born Green Generation's key partners - is an important step towards reducing single-use waste and promoting a greener healthcare system.
How did single-use become the default?
Historically, the healthcare sector relied almost exclusively on reusable medical devices made from durable materials like stainless steel, designed to be sterilised and used multiple times. However, driven by trends in the broader economy, the rise of disposable plastics led the industry to embrace single-use devices. These were marketed as safer alternatives, particularly for preventing healthcare-associated infections (HAIs). While this has undoubtedly been the case for certain items, such as syringes, this shift has entrenched a 'single-use' mentality across the sector. As a result, many devices with the potential to be safely sterilised have become disposable for the sake of convenience.
The often false claims of ‘single-use’
The term 'single-use' applied to medical devices can be misleading. Since manufacturers, not regulators, determine whether a device is labelled as single-use, this classification can be influenced by a number of factors, including marketing, liability concerns and the additional cost of validating a device for reuse, rather than simply the durability of the materials.
Many medical devices, including thermometers, blood pressure cuffs, and even more expensive equipment, such as endoscopes, are made of durable materials and are often sterilisable and can be safely reused. However, they are usually thrown away after one use, simply because of their label. Not only does this practice create unnecessary waste, it also increases healthcare costs, putting further strain on healthcare systems.
Reprocessing offers a sustainable solution, particularly for high-cost items. When done according to strict guidelines, reprocessed devices can be as safe as new ones. This practice provides hospitals with an effective, cost-saving method to reduce waste and mitigate supply chain issues. However, the lack of clear legislation has historically been a barrier to its widespread adoption across the EU.
Denmark's path to legalising reprocessing
On January 1 2025, Denmark will legalise the reprocessing of medical devices, marking a significant step towards more sustainable healthcare practices. This decision follows a comprehensive, multi-year process that began with Aarhus University Hospital, one of the country’s largest and most respected medical institutions. Prior to the introduction of the Medical Device Regulation (MDR), the hospital had collaborated with a German reprocessing service. However, when the MDR came into effect in 2021, a legal barrier emerged: without national legislation, the hospital could no longer access these services.
In response, Aarhus University Hospital partnered with the Centre for Sustainable Healthcare to drive a structured process to create a regulatory framework for reprocessing in Denmark. This initiative included extensive stakeholder consultations and expert assessments, culminating with the formation of a working group in October 2021. The group evaluated the safety, practicality, and potential benefits of reprocessing single-use medical devices, considering economic, supply chain, and environmental factors. The deliberations of the working group and the various public consultations that were held formed the basis for the final decision of the Ministry of Health to allow reprocessing in Denmark. Health Care Without Harm Europe also contributed to this process by responding to the final public consultation in support of the decision.
The benefits: Reduced cost, environmental impact and supply chain security
The findings of the Danish working group highlight the significant benefits of reprocessing single-use medical devices. In financial terms, the cost savings are considerable, with estimates ranging from 30 to 59 percent (1, 2, 3). According to the working group's calculations using a formula from a preliminary study, Aarhus University Hospital could save up to €330,000 per year on ultrasound catheters, and findings from Sweden suggest that local reprocessing of certain devices could lead to savings of around €5.8 million per year.
From an environmental perspective, reprocessing offers a tangible way to reduce the carbon footprint of healthcare. Aarhus University Hospital reported a 56% reduction in CO₂ emissions for reprocessed ultrasound catheters. Reprocessing also reduces dependence on virgin plastics and other raw materials, directly addressing key sustainability challenges.
Safety remains a priority. The Danish Infection Control Unit confirmed that reprocessing can be carried out safely if strict guidelines are followed, with careful evaluation of devices and compliance with EU regulations. However, they raised concerns about under-reporting of complications and challenges in attributing problems to reprocessed devices, highlighting the need for robust monitoring and reporting systems.
Reprocessing also strengthens supply chain security by ensuring a reliable supply of essential medical devices, particularly during global crises such as the COVID-19 pandemic. The Working Group noted that by reducing reliance on new (often foreign) manufacturing and diversifying sources of critical devices, health systems can better withstand disruptions and maintain patient care in challenging circumstances.
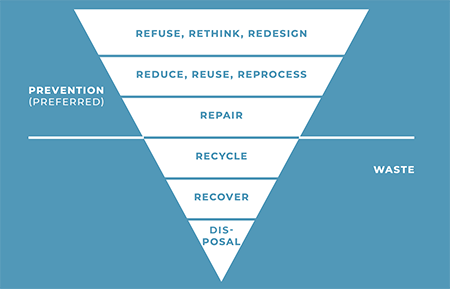
Beyond reprocessing: A vision for Circular Healthcare
While reprocessing is a significant step forward, it is only part of the solution. Achieving a truly circular healthcare system requires rethinking device design from the outset. Manufacturers must prioritise the development of durable, multi-use medical devices to reduce the sector’s dependency on unnecessary single-use items. Collaborative efforts between Danish hospitals and device manufacturers could catalyse innovation and advocate for regulatory frameworks that support reusable designs, fostering long-term sustainability.
The UK has taken a notable step in this direction with its Design for Life roadmap, announced in October. This initiative aims to phase out all unnecessary single-use items in the NHS by 2045. Policies like this are critical to addressing the entrenched single-use mindset in the healthcare sector. However, for these actions to be successful, the commitment must go beyond the efforts of any one country or health system. European policymakers must reshape the regulatory landscape on a broader scale to enable and encourage these systemic changes, laying the foundations today for meaningful progress towards a circular healthcare system in the near future.
Reprocessing represents a crucial milestone in the journey towards a greener healthcare system. By adopting a robust reprocessing framework, Denmark can address both environmental and economic challenges while maintaining the highest standards of patient care. This policy shift offers a clear roadmap for other nations, demonstrating how healthcare can lead the way in the transition to a circular economy.