Blog by Viktor Jósa, Climate Policy & Projects Officer
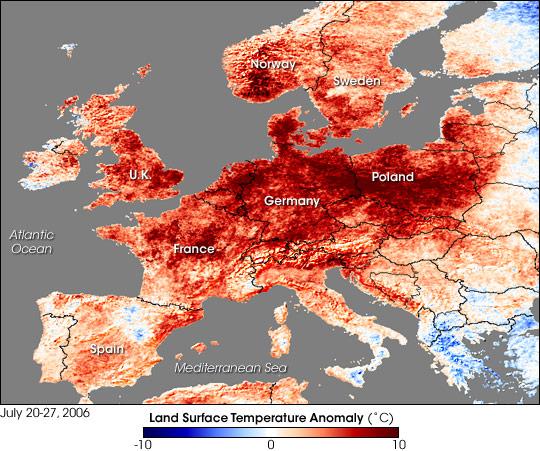
After a summer of extreme weather in Europe that has brought scorching heat to Britain, drought to the Netherlands and blazing wildfires to Greece, the heatwave affecting different parts of Europe has presented challenges for healthcare institutions. Rather than once-in-a-lifetime events, however, these extremes may become the “new normal” as a result of climate change and rising global temperatures affecting weather patterns. Evidence is emerging from the analysis of long-term climate records about an increase in the frequency and duration of extreme heatwaves. Climate modelling studies indicate that summers such as the one we have just experienced in Europe, as well as the heatwave of 2003, may well offer a taste of what is to come for Europe in the latter part of the 21st century.
The threats that heatwaves pose to the health sector include those to the health of the population, those that threaten the delivery of services through changes in service patterns, and infrastructural challenges. Exceptionally hot days can also cause the overheating of hospital buildings and lead to increased risks of ambient air pollution and its associated health effects.
Urban centres (where most hospitals are located) also experience heatwaves more drastically, because of the heat island effect, which occurs when heat is stored in the urban infrastructure during the day, only to be slowly released during the night, with no cooling evaporation. During heatwaves this results with night time urban temperatures several degrees above those outside the city.
The National Health Service (NHS) in the UK laid out its plans to address the risks associated with climate variability in their Health and Care System Adaptation Report, part of the National Adaptation Programme (NAP). The health sector in England has set objectives to ensure the health system is resilient in the face of climate change. These objectives include:
- To reduce mortality and morbidity associated with severe weather events and climate change.
- To promote resilience and service continuity to ensure sound service delivery.
A number of national plans are also in place to support these objectives - the UK government has well-established heatwave and cold weather plans which will also help the sector prepare for and respond to extreme weather events. The NHS itself has been rolling out heatwave plans annually since 2004, following the unprecedented pan-European heatwave in 2003, which caused more than 70,000 excess deaths across 12 European countries.
Healthcare practitioners tend to think that the winter months are the most challenging for the sector. If current trends continue, however, the sector will face climate-related health challenges all year round.
Contrary to deaths associated with cold snaps in winter, mortality as a result of very warm weather is very closely linked to temperature, and mortality rises within one or two days of the temperature rising. For the health sector this means that, by the time a heatwave starts, the window of opportunity for effective action is very short.
The UK’s heatwave plan outlines what should happen before and during periods of severe heat. It sets out how both individuals and organisations can prepare in order to reduce health risks (including specific measures to protect at-risk groups). Despite this preparedness, Britain’s extreme weather this summer still caused unexpected deaths, especially amongst the most vulnerable. In the seven weeks up until the end of July 2018, 1,000 more people died than predicted. According to MP Mary Creagh, Chair of the Environmental Audit Committee, excess mortality during the summer period could rise to anywhere between 4,000 and 14,000 a year if there are no steps taken to make cities and buildings safer. Creagh believes it’s a problem that is falling between the cracks, which is why some groups are calling for a minister to be appointed specifically to deal with heatwaves.

According to some NHS Trusts, the recent heatwave has meant that they’re facing winter conditions in hospitals, as well as in community, mental health and ambulance services. The UK’s hospital wards, along with many hospitals throughout Europe, struggle with indoor temperatures during heatwaves due to the lack of air conditioning in older buildings - turning healing environments into boiler rooms, where staff suffer from dehydration during long working shifts in temperatures exceeding 30°C.
Resilience = Increased immunity
It is virtually certain that the length, frequency and intensity of heatwaves will increase in the future. This increase could lead to a substantial increase in mortality over the next decades, especially in vulnerable groups, unless measures are taken to improve the resilience of health systems. If not, hospitals and health systems in Europe will undoubtedly incur high costs resulting from the growing number of extreme weather events.
There is an unavoidable need to build health systems and facilities that withstand extreme weather events, while at the same time moving towards more climate-smart healthcare in order to achieve more equitable access to care.
For healthcare infrastructure to be resilient in the face of extreme weather, a set of adaptation measures related to building design and planning are necessary. Many resilience strategies also contribute to climate change mitigation and vice-versa. For example, designing buildings with natural ventilation, developing on-site energy generation (including solar and other renewable sources), combined heat and power systems, and purchasing energy-efficient medical devices are some of the measures that contribute to both health system resilience and carbon footprint reduction.
While Europe is experiencing intense heatwaves that are challenging healthcare services, awareness is raising among hospitals and health systems about the need to develop climate-smart solutions. Many hospitals have already accelerated healthcare’s move towards decarbonisation, increased their resilience, and mobilised leadership to combat climate change.
Climate-smart healthcare has to become a basic pillar of sustainable development, and HCWH can provide invaluable support for those seeking to set targets for mitigation, resilience, and leadership, as well as measure progress towards sustainability goals through the Health Care Climate Challenge. It's possible to confront this new climate normal and the health sector can become a leader in early mitigation in times when opportunities are being lost with every decade that emissions rise. Now is the time for the healthcare sector in Europe to lead from the front in mitigating its own climate footprint, become more resilient in the face of extreme weather events, and show true leadership in tackling climate change - which, as The Lancet outlines, is the “greatest global health opportunity of the 21st century.”