
A blog post by Andreea Zotinca, Circular Healthcare Project Officer – HCWH Europe
Medical protective clothing is essential not only to protect medical professionals from pathogens, but also to protect patients from possible contamination. Surgical masks, respirators, gowns, aprons, gloves, and visors have become indispensable in the fight against the COVID-19 virus, yet this increase in consumption and disposal of single-use products is negatively impacting our environment and health.
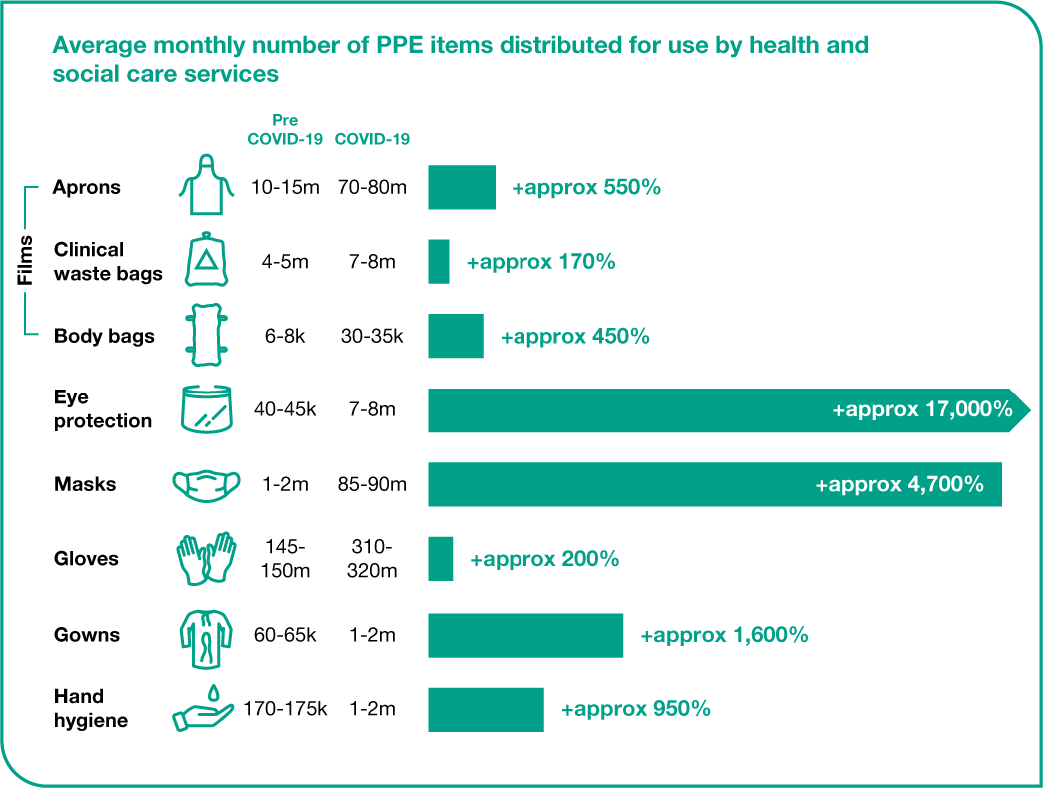
During the pandemic, the UK healthcare sector alone has seen demand for facemasks grow by 4,700% - up to 85-90 million per month. Similarly, the consumption of single-use aprons and gloves has grown 550% and 200% respectively. This trend is not unique to the UK and the skyrocketing growth of disposable medical protective clothing is increasingly problematic.
The impact of disposable medical protective clothing
The excessive production of disposable medical protective clothing undermines our health and climate goals – the majority are made from plastic, which continues our reliance on fossil fuels, especially at the current scales of production. After a short, single-use life, disposable medical protective clothing also continues to harm the environment and our health through disposal:
- Incineration - generates further carbon emissions, as well as toxic gases such as dioxins or furans, and toxic ashes
- Landfill – products can persist for hundreds of years, potentially leaching toxic chemicals to soil and water
Some hospitals might consider single-use bio-based options, but they are not necessarily better for the environment and do not address the fundamental issues surrounding our consumption behaviour.
Protective clothing and PPE are not the only single-use plastics used in healthcare that can be reduced and replaced, learn more in our project Towards plastic-free healthcare in Europe.
The social aspect of linear production models is often overlooked - plastic manufacturing facilities, as well as incineration sites and landfills, are often in close proximity to deprived communities, putting their health at further risk. The production of medical protective clothing, as with many other global supply chains, is also linked with workers’ rights violations and alarming working conditions.
Supply shortages in a crisis

During shortages, many healthcare workers have had no choice but to reuse items that were meant to be disposable - out of necessity, they found ways to sterilise single-use N95 respirators with vaporised hydrogen peroxide for example.
Decontamination of single-use protective clothing is only an emergency practice, however, and does not solve the shortage crisis. Hospital management and procurers should focus efforts on adopting alternative, safe and reusable protective clothing; where reusable alternatives are not yet available, procurers should ensure that products meet environmental and social criteria, and support innovation towards more durable, reusable items. Healthcare procurers should also read the European Safety Federation’s Reflections on sustainability of PPE, which offers many recommendations that can also be applied to most medical protective clothing.
The NHS started a pilot project in the UK to introduce reusable IIR certified face masks, showing how healthcare can promote demand for reusable products in a market otherwise dominated by disposables. There are remaining regulatory challenges, but this pilot shows a lot of potential and could represent significant progress in the move away from our disposable culture.
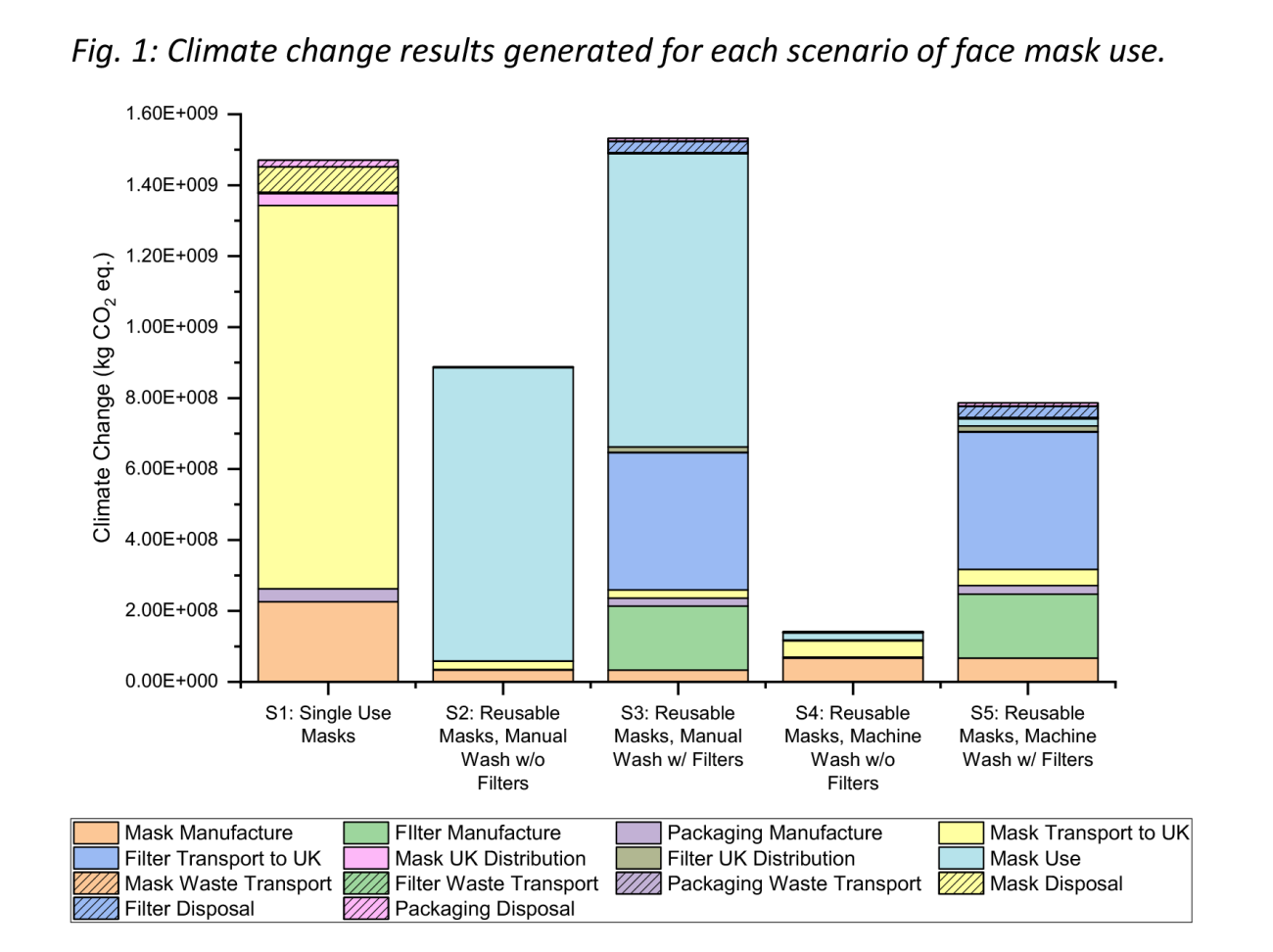
[Image: UCL Plastic Waste Innovation Hub (2020) The environmental dangers of employing single-use face masks as part of a COVID-19 exit strategy]
The challenges and benefits of reusable protective clothing in healthcare
Challenges
Transitioning to reusable medical protective clothing provides many opportunities but there are often barriers that must be considered.
1. Contamination fears
A common argument in favour of disposable items in healthcare is the simplification that disposables reduce contamination risk and reusables increase it. Infection risk, however, is highly dependent on the product and the procedure, as well as many other factors – a more thorough analysis is therefore needed. It is difficult to demonstrate that specific disposable products provide a reduced infection rate and the perceived higher infection risk associated with reusable items is either not demonstrated or extremely small.
Many recent studies unfairly compare disposable surgical face masks with reusable, ‘homemade’ cotton ones, instead of medical grade reusable masks. Surgical masks were reusable until the 1960s and did not pose infection prevention and control issues, with studies at the time attesting for their quality and even the superiority of fabric masks. Large-scale production of medical grade reusable masks stopped and it is now difficult to conduct new studies on them.
Recent progress in reducing surgical site infection rates is not necessarily associated with disposables, but rather care standardisation and improvements in host defence mechanisms. Hygiene experts have observed that there is no significant difference in infection risk between clean disposables and well sterilised reusables.
2. Logistics and ease of current practices
One common problem is that many hospitals closed their on-site cleaning and sterilisation facilities in the transition to disposables, meaning they do not have the capacity to support reusable protective clothing in-house anymore. If reopening those facilities is no longer feasible, external providers can be an alternative. Other logistical aspects also need to be considered, such as storage space, tracking number of uses, and changes in staff behaviour.
Benefits
When switching to reusables it is crucial to involve all stakeholders and have leadership support to ensure a successful transition – this can be supported by a number of co-benefits.
1. Cost savings
Using gowns as an example, whilst a single disposable gown is cheaper than a reusable one, when you look at the whole-life-cost, reusables are cheaper in most cases. For an accurate cost comparison, the cost of waste disposal, cleaning, and cost per use need to be considered. Cost-savings can be significant - UCLA Health in the US, has so far saved more than $3 million USD - an average of $450,000 per year.
2. Building resilience
Environmental and climate risks are growing and it is crucial that our healthcare systems are resilient and can continue delivery of care. Adopting reusable medical protective clothing, thus ensuring an inventory of protective clothing is always available, can help avoid supply shortages similar to those we have seen during COVID-19. Many healthcare facilities have adopted reusable gowns to cope with the single-use supply chain shortages, but a more developed market for reusables is needed to continue; procurers can use their influence to demand reusable alternatives.
3. Environmental improvements
Reusable medical protective clothing reduces waste and, when production is compared, disposable textiles have a 200–300% larger carbon footprint as well as increased energy, water, and resource consumption. Further advances in cleaning technology also mean that the water and energy use for cleaning reusables is decreasing.
4. Safer chemicals
Medical textiles, widely used in protective clothing, often contain chemicals hazardous to health and the environment. As more healthcare providers explore reusable solutions, there is a significant opportunity to carefully consider the materials and chemical substances used in the production and treatment and support a toxic-free environment. The Central Denmark Region, for example, is making efforts to ensure that hazardous chemicals such as PFAS are not used in their reusable gowns.
Healthcare practitioners and hospital managers need to recognise the growing environmental problems linked to single-use items and take steps to protect the health of people and the planet wherever they can. Reusable medical protective clothing offers significant advantages: increased healthcare resilience, a smaller environmental footprint, and lower costs – all of which benefit patients and public health. The healthcare sector has the leverage and the influence to lead the transition to reusables whenever they are available and demand for sustainable innovations when they are not.
Break Free From Plastic (BFFP) has launched the #WeChooseReuse campaign to encourage the implementation of reuse systems and disrupt our overreliance on single-use plastics. While some single-use plastic items remain necessary in healthcare applications, the COVID pandemic has exposed the sector’s overreliance on them and has further highlighted the need to transition to reusable systems.
The healthcare sector has the moral responsibility and the influence to transform how we deliver care. By reducing the environmental impact of the sector through innovation, a circular economy, and powerful advocacy we can create a sustainable healthcare sector, that is good for the planet and for the patient.
